Definition of radiotherapy in physics
Radiotherapy, also known as radiation therapy, is a medical treatment that uses ionizing radiation to kill cancer cells and shrink tumors. It is a branch of medical physics that utilizes high-energy radiation, such as X-rays or gamma rays, to deliver targeted doses of radiation to the affected areas of the body.
Radiotherapy works by damaging the DNA within cancer cells, preventing them from dividing and growing. The radiation damages the genetic material of cancer cells, leading to cell death or impairing their ability to multiply. This helps to control or eliminate the cancerous growth.
Radiotherapy can be performed externally or internally. External beam radiotherapy involves aiming high-energy X-rays or gamma rays at the tumor from outside the body using specialized machines, such as linear accelerators. Internal radiotherapy, on the other hand, involves placing radioactive materials directly into or near the tumor.
The planning and delivery of radiotherapy are highly precise and tailored to each patient’s specific condition. Medical physicists, along with radiation oncologists and radiation therapists, work together to create a treatment plan that maximizes the radiation dose to the tumor while minimizing the exposure to surrounding healthy tissues.
Radiotherapy is used as a primary treatment for various types of cancer, as well as in combination with surgery or chemotherapy. The goal of radiotherapy is to eradicate cancerous cells, control tumor growth, alleviate symptoms, and improve the patient’s quality of life.
Principles and techniques of radiotherapy
Principles and techniques of radiotherapy:
1. Principle: Radiotherapy uses ionizing radiation to target and kill cancer cells, while minimizing damage to surrounding healthy tissues.
2. Techniques: There are several techniques used in radiotherapy, including:
– External Beam Radiotherapy (EBRT): This is the most common form of radiotherapy, where a linear accelerator delivers radiation beams from outside the body to the tumor. Different techniques within EBRT include 3D conformal radiotherapy, Intensity-Modulated Radiotherapy (IMRT), and Stereotactic Radiosurgery (SRS) or Stereotactic Body Radiotherapy (SBRT).
– Brachytherapy: This technique involves placing radioactive sources inside the body, close to or within the tumor. It can be used for various tumor types, including gynecological, prostate, and head and neck cancers.
– Proton Therapy: Proton beams, which have different physical properties compared to conventional photon beams, are used to deliver radiation to tumors. Proton therapy is particularly useful in tumors located near critical structures.
– Particle Therapy: This includes the use of heavier charged particles like carbon ions or helium ions to deliver radiation to tumors. Particle therapy is advantageous in certain tumor types and locations, as it can provide better dose distribution and spare normal tissues.
3. Treatment Planning: Before radiotherapy, a thorough treatment plan is created. This involves imaging the tumor, mapping and defining the target area, and determining the optimal radiation dose and treatment regimen. Advanced software systems are used to generate treatment plans based on the specific characteristics of the tumor and normal tissues.
4. Treatment Delivery: Once the treatment plan is finalized, radiotherapy sessions are scheduled. The patient is carefully positioned on the treatment machine, and radiation beams are delivered according to the treatment plan. Treatment sessions are usually repeated over a period of days, weeks, or months, depending on the specific treatment protocol.
5. Quality Assurance: Radiotherapy requires stringent quality assurance procedures to ensure accurate dose delivery and patient safety. This includes regular checks and calibrations of treatment machines, verification of treatment plans, and precise patient positioning.
6. Side Effects: Radiotherapy can cause both acute and long-term side effects. Acute side effects may include fatigue, skin reactions, and temporary hair loss. Long-term side effects depend on the treated area and dose received and may include organ dysfunction or secondary cancers. Close monitoring and supportive care are crucial to manage and minimize these side effects.
Overall, radiotherapy plays a critical role in cancer treatment, either as a standalone treatment or in combination with surgery or chemotherapy. The principles and techniques of radiotherapy continue to evolve, with advances in technology and research contributing to improved outcomes for patients.
Applications of radiotherapy in cancer treatment
There are several applications of radiotherapy in cancer treatment. Radiotherapy involves using high-energy X-rays or other types of radiation to kill or shrink cancer cells. It plays a crucial role in the overall management of cancer and may be used as the primary treatment or in combination with other therapies. Some of the main applications of radiotherapy in cancer treatment include:
1. Curative treatment: Radiotherapy can be used with the aim of curing cancer, particularly in early-stage cases. It is often used as the primary treatment modality for localized tumors, such as in breast, lung, prostate, and cervical cancer. The radiation is carefully targeted to the tumor site, delivering doses that are sufficient to eradicate cancer cells while minimizing damage to healthy surrounding tissues.
2. Adjuvant treatment: Radiotherapy may be used after surgery to eliminate any remaining cancer cells that may not have been completely removed during the surgical procedure. This helps reduce the risk of cancer recurrence. This approach is commonly used in breast, prostate, and colorectal cancer.
3. Palliative treatment: In cases where cancer has spread or is in advanced stages, radiotherapy can be used to relieve symptoms and improve quality of life. Palliative radiotherapy is often used to shrink tumors that are causing pain, bleeding, or obstructing vital structures. For example, it can be used to reduce pain in bone metastases or to alleviate symptoms associated with brain tumors.
4. Neoadjuvant treatment: Radiotherapy can be administered prior to surgery or other treatments to reduce the size of tumors and make them more operable. It is particularly useful in certain types of localized cancer, such as rectal cancer, where shrinking the tumor before surgery can improve the chances of successful removal.
5. Prophylactic treatment: In certain high-risk groups, such as individuals with a genetic predisposition to certain cancers, radiotherapy can be used as a preventive measure. This is often the case in individuals at high risk of breast or ovarian cancer due to BRCA gene mutations, where prophylactic mastectomy or oophorectomy may be combined with radiotherapy.
6. Combined modality therapy: Radiotherapy is often used in combination with other treatment modalities, such as surgery, chemotherapy, or targeted therapy. This multimodality approach can help improve treatment outcomes and increase the chances of complete cancer eradication. Combinations like chemoradiotherapy are commonly used in lung, head and neck, and esophageal cancer.
It is important to note that the use of radiotherapy in cancer treatment is highly individualized. The specific treatment approach depends on factors such as cancer type, stage, location, patient’s overall health, and treatment goals. Radiotherapy can be delivered through external beam radiation therapy, brachytherapy, or systemic radioactive drugs, and the treatment plan is tailored to each patient’s unique needs.
Benefits and limitations of radiotherapy
Benefits of radiotherapy:
1. Effective at killing cancer cells: Radiotherapy uses high-energy radiation to target and destroy cancer cells. It can be highly effective in treating various types of cancer, including breast, lung, prostate, and brain cancer.
2. Non-invasive treatment: Unlike surgery, radiotherapy is a non-invasive treatment option. It does not require incisions or the removal of tissue, which can lead to quicker recovery times and reduced risk of complications.
3. Can be used in combination with other treatments: Radiotherapy can be used alongside other cancer treatments, such as chemotherapy or surgery, to increase the effectiveness of treatment. It is often used before surgery to shrink tumors or after surgery to destroy any remaining cancer cells.
4. Precise targeting: Modern radiotherapy techniques have advanced targeting systems, such as image-guided radiation therapy (IGRT) or intensity-modulated radiation therapy (IMRT), that allow for the precise targeting of cancer cells while minimizing damage to healthy tissues.
5. Pain relief: Radiotherapy can be used to shrink tumors that are causing pain or other symptoms, providing relief and improving the quality of life for patients.
Limitations of radiotherapy:
1. Damage to healthy tissues: Although modern techniques aim to minimize damage to healthy tissues, radiotherapy can still cause side effects. These can include fatigue, skin irritation, hair loss, and damage to nearby organs.
2. Non-specific targeting: While efforts are made to target cancer cells, radiotherapy cannot distinguish between cancerous and healthy cells entirely. This may lead to damage to some healthy tissues in the irradiated area.
3. Potential long-term side effects: Some side effects of radiotherapy, such as radiation fibrosis or secondary cancers, may develop years after treatment. These long-term side effects need to be carefully monitored.
4. Limited effectiveness for advanced stages: Radiotherapy may not be as effective for advanced-stage cancers or cancers that have spread to distant sites in the body. In these cases, other treatment options, such as chemotherapy or targeted therapy, may be more suitable.
5. Availability and accessibility: Not all healthcare facilities have the resources or expertise to provide advanced radiotherapy treatments. This can limit access to radiotherapy for some patients, particularly those in remote areas.
Future developments in radiotherapy
There are several exciting future developments in radiotherapy that hold promise for improving treatment outcomes and patient experiences. Some of these developments include:
1. Advanced imaging techniques: Imaging plays a crucial role in radiotherapy treatment planning and targeting tumors. Future advancements will focus on integrating new imaging modalities such as magnetic resonance imaging (MRI) and positron emission tomography (PET) into the radiotherapy workflow. This will provide more accurate and precise imaging of tumors, helping to tailor treatment plans to individual patients.
2. Adaptive radiotherapy: The ability to adapt treatment plans in real-time based on changes in tumor size, shape, or position during treatment is a major focus of research. This approach, known as adaptive radiotherapy, allows for personalized treatment that can effectively target the tumor while minimizing damage to surrounding healthy tissues.
3. Proton therapy: Proton therapy is a type of radiation therapy that uses protons instead of traditional X-rays to deliver treatment. Protons have different physical properties than X-rays, allowing for more precise targeting of tumors and potentially reducing side effects. Proton therapy is currently being studied and implemented in more clinics, with ongoing advancements in technology to make it more accessible and affordable.
4. Immunotherapy combination: Radiotherapy has been shown to have immunomodulatory effects by enhancing the body’s immune response against tumors. Future developments will focus on combining radiotherapy with immunotherapies, such as checkpoint inhibitors, to further enhance the immune system’s ability to recognize and attack cancer cells. This combination approach has the potential to improve treatment outcomes and increase the efficacy of radiotherapy.
5. Enhanced patient experiences: Future developments in radiotherapy will also focus on improving patient experiences during treatment. This includes advancements in imaging and treatment delivery technologies to reduce treatment times, increase comfort, and minimize side effects. Additionally, advancements in patient positioning and immobilization techniques will help ensure accurate and reproducible treatment delivery.
Overall, future developments in radiotherapy aim to provide more personalized and effective treatments, with reduced side effects and improved patient experiences. These advancements hold great potential for advancing cancer care and improving outcomes for patients undergoing radiotherapy.
Topics related to Radiotherapy
Dosimetry: fundamentals II – YouTube
Dosimetry: fundamentals II – YouTube
Radiotherapy: how does it work? – YouTube
Radiotherapy: how does it work? – YouTube
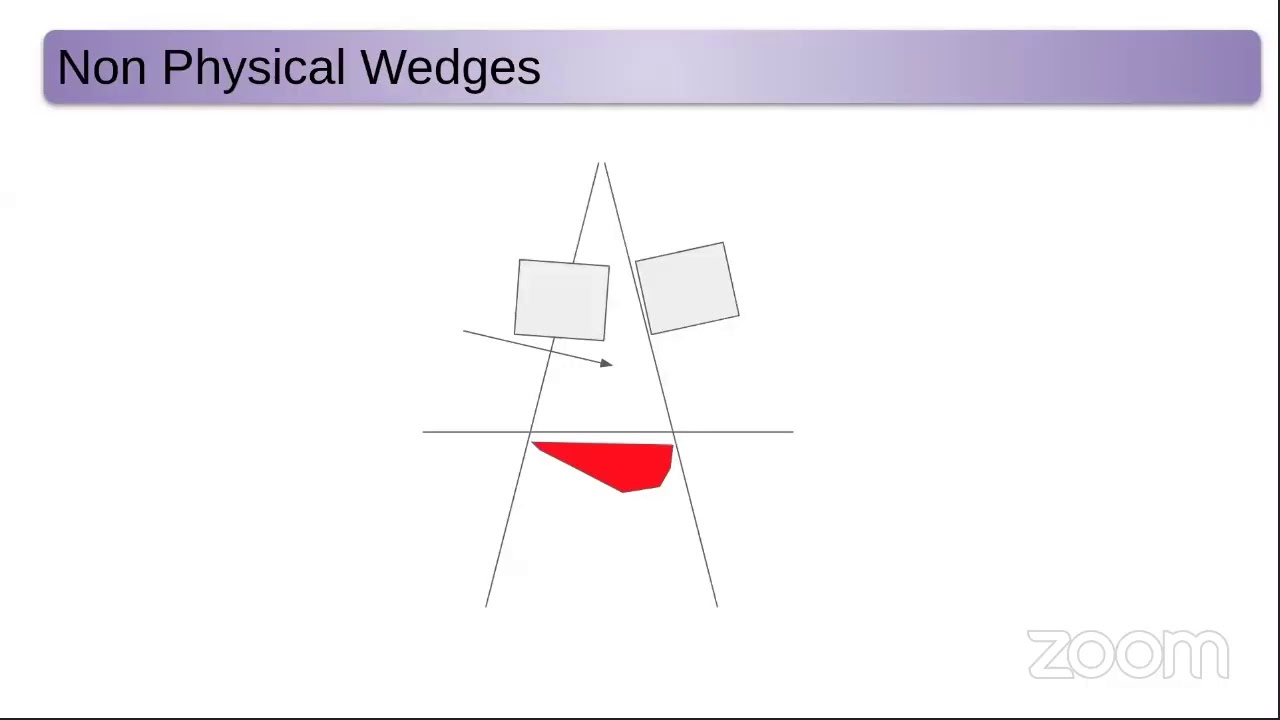
Radiotherapy Physics webinar – YouTube
Radiotherapy Physics webinar – YouTube
Healthcare Science Week 2023 | Radiotherapy Physics – YouTube
Healthcare Science Week 2023 | Radiotherapy Physics – YouTube
Cancer Treatment: IMRT (Radiation Therapy) – YouTube
Cancer Treatment: IMRT (Radiation Therapy) – YouTube
Radiation Oncology Medical Physics Residency: Preparing Future Physicists – YouTube
Radiation Oncology Medical Physics Residency: Preparing Future Physicists – YouTube
Medical Physics Class _9(Young Radiation Oncologists" Club ) – YouTube
Medical Physics Class _9(Young Radiation Oncologists" Club ) – YouTube
How Radiotherapy Works! – YouTube
How Radiotherapy Works! – YouTube
Physics of Radiation treatment of cancer – YouTube
Physics of Radiation treatment of cancer – YouTube
Radiotherapy | 9-1 GCSE Physics | OCR, AQA, Edexcel – YouTube
Radiotherapy | 9-1 GCSE Physics | OCR, AQA, Edexcel – YouTube

Konstantin Sergeevich Novoselov is a Russian-British physicist born on August 23, 1974. Novoselov is best known for his groundbreaking work in the field of condensed matter physics and, in particular, for his co-discovery of graphene. Novoselov awarded the Nobel Prize in Physics. Konstantin Novoselov has continued his research in physics and materials science, contributing to the exploration of graphene’s properties and potential applications.